During the COVID-19 pandemic, the use of face masks increased dramatically due to health directives both in Australia and overseas. But now that the pandemic is over and governments around the world have removed mask mandates, do we still need to wear face masks?
Read on to understand the benefits of face masks and the different scenarios when wearing a face mask could be useful.
When should I wear a face mask?
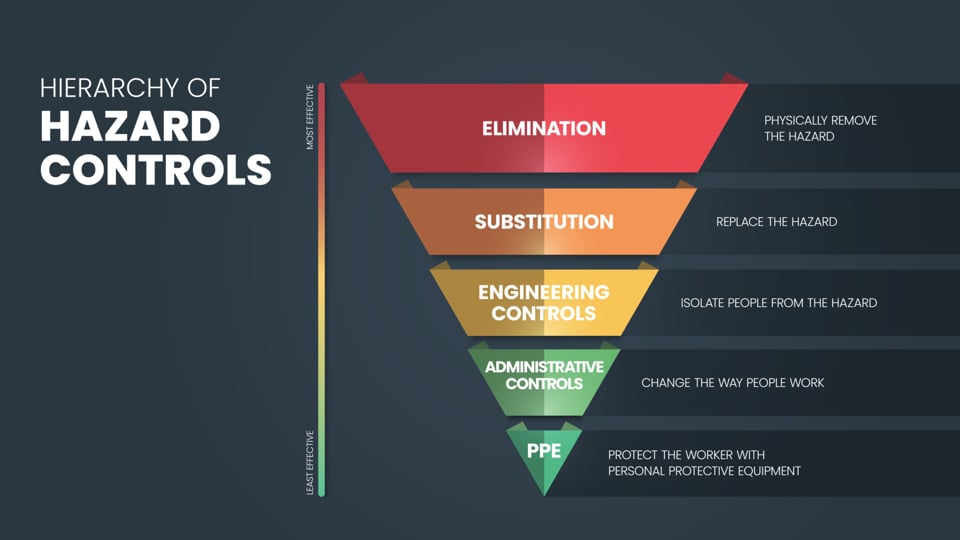
As a key element within the hierarchy of controls, face masks and respirator masks are a requirement under several workplace health and safety standards, including the National Safety and Quality Health Service Standards. That said, there are a number of instances both within and outside of healthcare settings where face masks and respirators provide much-needed respiratory protection.
Here are some of the situations where it’s often worth wearing a face mask.
During outbreaks of respiratory illnesses
From time to time, Australia experiences outbreaks of different respiratory viruses. While these outbreaks often aren’t on the same scale as the COVID-19 pandemic, face masks can help to provide respiratory protection and reduce the spread of infection.
For example, face masks are often recommended during flu season to help curb the number of cases. Plus, masks can often provide effective protection against other influenza-like illnesses, like rhinovirus or the common cold.
Earlier this year, several states around Australia recorded confirmed cases of avian influenza. As a result, the government departments, including NSW Health, strongly recommended that animal professionals and individuals responding to the outbreak wear an P2 N95 Respirator Mask (P2 D95 Respirator Mask) at a minimum to protect against human transmission.
In healthcare settings
While there are no current public health directives mandating the use of face masks, you might still be asked to wear a face mask in certain healthcare settings. Hospitals, clinics, aged care settings and other long-term care facilities often still recommend or require masks to protect vulnerable patients and healthcare workers from potential infection.
To protect against dust and smoke
Although face masks are often used as protection against viruses and infectious diseases, they also play a key role in protecting people from dust, smoke and other hazardous particles. With this in mind, masks and other respiratory protection are often a workplace health and safety requirement in construction and mining environments, where workers are at higher risk of exposure to these types of airborne particles.
If you’re unwell
Face masks don’t just provide protection for the wearer. Certain types of masks can also prevent the spread of infection if you’re feeling under the weather. This is often referred to as source or infection control.
In particular, surgical respirators are made with several inner layers of fabric that are designed to capture the wearer’s respiratory droplets and secretions, helping to reduce the risk of transmission.
If you’re suffering from allergies
By design, face masks and respirators are made from multiple layers of lightweight materials that capture droplets, bacteria and other particles. By acting as a physical barrier, masks and respirators can also protect against the inhalation of allergens, like pollen, dust mites, pet dander and mould spores.
By blocking these particles from entering the respiratory system, masks and respirators can often help to alleviate the symptoms of allergies. Similarly, masks and respirators are also ideal for use in environments with poor air quality or high levels of air pollution.
Which mask should I choose?
Different masks offer varying levels of protection. With this in mind, the best face mask often depends on the circumstances and your individual needs.
Here’s a quick breakdown of some of the most common face masks to choose from.
3-Ply community face masks
Community face masks are designed to provide protection in settings where physical distancing isn’t possible, making them ideal for retail, food service and event settings.
Level 2 medical procedure face masks
Medical masks provide protection against blood or fluid splash, so they’re typically recommended for use in clinical settings.
Level 3 surgical face masks
If you’re after a little extra protection, level 3 surgical face masks are designed for use where a person is at risk of blood or fluid splash. They’re ideal for protecting against sneezes and coughs from other people while also offering a form of source control by capturing the wearer’s bodily droplets.
Respirator masks
For protection in high-risk settings, respirator masks are your best bet. These masks offer the highest level of filtration, blocking up to 95% of airborne particles, including fine aerosols. They are recommended in high-exposure settings or for people at greater health risk. Respirator masks are also available in several options offering varying levels of protection. From N95 surgical respirator masks to level 3 N95 surgical respirators, these masks can be used in community settings, industrial environments and in the healthcare sector.
Stock up on masks with Detmold Medical
Detmold Medical is home to a wide range of face masks and respirators for use in healthcare, retail, hospitality, and community settings. To find the best face mask for your environment or needs, use our Face Mask Comparison Guide or shop the range online.





