Infection prevention is essential for protecting the health and wellbeing of vulnerable patients and workers within healthcare settings. Not to mention, implementing effective infection prevention and control systems is a requirement under the National Safety and Quality Health Service (NSQHS) Standards. That’s where the hierarchy of control comes in.
Read on to learn more about how to apply the hierarchy of control to prevent the spread of infections in healthcare settings.
What is the hierarchy of control?
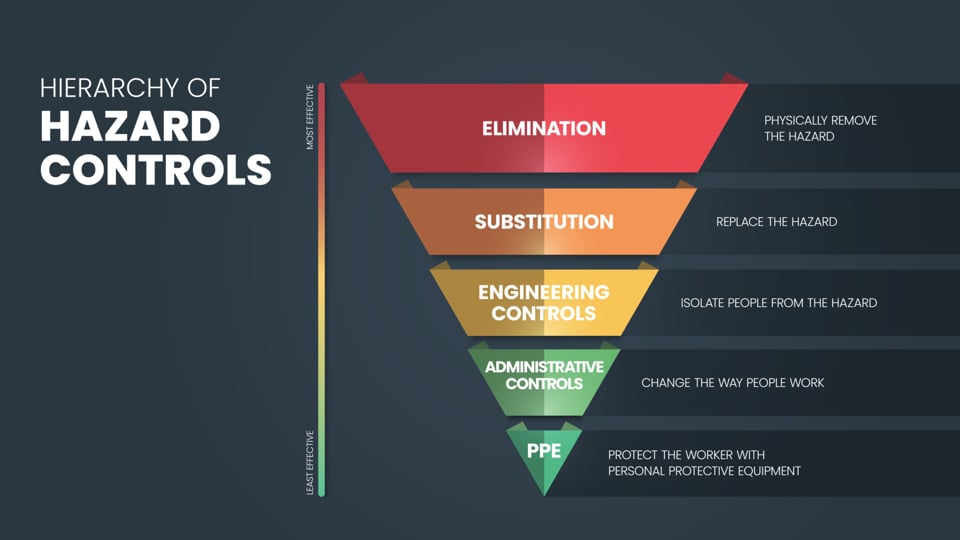
The hierarchy of control is a system that’s used to control risks and hazards in the workplace. This approach is used across various industries, including mining and construction. It’s also frequently implemented in hospital and healthcare environments to prevent the spreading of infections and viruses.
It provides a step-by-step approach to eliminate or minimise hazards from the most effective controls to the lowest level of protection. The hierarchy of control can be split into six different categories.
Before applying the hierarchy of control, it’s essential to complete a risk assessment to identify potential hazards that could impact the workplace. A risk assessment involves:
1. Identifying hazards involves identifying potential hazards that could cause harm, like infectious agents, contaminated surfaces, or unsafe procedures in a healthcare setting.
2. Assessing risks determines their likelihood and potential severity.
3. Controlling risks is where the hierarchy of control comes into play. It involves taking steps to prevent the spread of infections.
4. Reviewing control measures involves evaluating how effective the controls are. If certain controls aren’t working, other controls should be implemented to ensure ongoing safety.
Let’s take a look at the six categories from most effective to least effective.
Elimination
Elimination is the most effective control method. It involves the complete removal of the infection risk. While eliminating the risk of infection might sound like a good approach in theory, in practice, it’s often impossible to remove the risk entirely.
For example, in hospitals, it’s next to impossible to completely eliminate pathogens, infections, and viruses, with patients constantly coming and going. That said, a typical example of elimination for infection prevention is discharging patients once they no longer need care, effectively removing the source of infection.
Substitution
Substitution is the process of replacing hazardous processes, materials, or pathogens with safer alternatives.
While this approach is less commonly applied directly to infection control in hospitals, it can be seen in practices like replacing older, riskier treatments with safer alternatives that carry lower infection risks. Another form of substitution is using less invasive techniques that reduce infection risk, like swapping open surgery for laparoscopic surgery instead.
Isolation
Isolation focuses on separating infected patients or high-risk areas from other parts of the hospital to prevent the spread of infection.
This is a critical part of infection control in healthcare settings and includes:
- Standard isolation procedures for patients with contagious diseases,
- Designated areas for high-risk activities (EG. operating theatres, infectious disease wards), and
- Using negative pressure rooms for airborne pathogens like tuberculosis (TB).
Engineering controls
Engineering controls focus on designing systems and infrastructure to reduce the risk of transmission. These controls protect both healthcare workers and patients by managing the environment.
Examples include:
- Ventilation systems to ensure adequate airflow, reducing the concentration of airborne pathogens,
- Barrier systems like plexiglass at nurse stations or reception areas,
- Automatic hand hygiene stations and touchless faucets, and
Sharps disposal systems to minimise the risk of needlestick injuries.
Administrative controls
Administrative controls involve the implementation of policies, protocols, and training programs aimed at reducing infection risk. These control measures are intended to manage the way people behave within healthcare and hospital settings.
Standard administrative controls include:
- Infection prevention protocols, such as hand hygiene programs and standard precautions,
- Workplace training on infection prevention and control measures and practices,
- Patient screening for infectious diseases upon admission,
- Vaccination policies for healthcare workers, and
- Workplace policies that limit the movement of staff and visitors in high-risk areas.
Personal protective equipment (PPE)
PPE is the last line of defence and involves wearing protective clothing and equipment to minimise exposure to infectious agents. It’s considered the least effective control measure because it relies on individual compliance, so it’s susceptible to user error.
When it comes to infection prevention, you’ll often find healthcare workers wearing:
- Gloves, face masks, gowns, and face shields for staff in contact with infectious patients,
- N95 surgical respirator masks for protection against airborne diseases, and
Eye protection for procedures that may generate splashes or sprays.
While PPE is typically worn by healthcare workers, face masks can also be worn by sick patients as a form of source control.
Infection prevention with Detmold Medical
As the Southern Hemisphere’s largest manufacturer of high-quality respirators and face masks, Detmold Medical is the supplier of choice for some of Australia’s largest government healthcare departments, hospital groups, and distributors. We offer a comprehensive mask range to suit a variety of different needs, from 3-ply community face masks to our new L3 N95 surgical tri-panel respirator masks.
But that’s not all. We also offer a range of other PPE and medical consumables to help with infection prevention in healthcare settings.
Get in touch with our specialist team to learn more about how Demold Medical can help prevent infections in your workplace or shop the range online.





